(Here are links to Parts 1, 2, 3, and 4)
Transitioning at Puberty:
When a child approaches puberty, the parents/guardians of a trans child, the child themself, and their GP or pediatrician will start having conversations about how they wish to approach the next phase. There would initially be 2 paths open to them:
Begin puberty blockers which delay the onset of puberty. The family, child, and GP may choose this option if there is a sense that the child wants or needs more time to explore their gender identity further, as well as giving time to plan for the psychological, medical, developmental, social, and legal issues that may lie ahead if they haven’t already done so. Puberty blockers are reversible, and a child may be on them for a couple of years. Transgender adolescents who have sought and received hormonal suppression as a part of a multidisciplinary approach to care report improved mental health and psychosocial functioning, and access to these medications has been associated with lower odds of suicidal ideation over the course of their life.
Begin hormone therapy. Gender-Affirming Hormone Treatment (GAHT) can begin after a transgender pre-adolescent has been on puberty blockers, and it can also occur if an adolescent has gone through puberty without puberty blockers. GAHT is prescribed to promote the development of physical features that are better aligned with an individual’s experienced gender, and can begin being administered at age 14. It’s considered a partially reversible intervention because it results in both reversible and irreversible changes. This is an important part of the transitioning process, as a 2021 peer-reviewed study found that gender-affirming hormone therapy is significantly related to lower rates of depression, suicidal thoughts, and suicide attempts among transgender and nonbinary youth.
The decision of which route to take is very personal and the adults (parents/guardians and medical doctor and oftentimes a psychologist) must center the well-being of the child in their discussion of these options. Since each trans child and situation is different, the choice is tailored to their specific needs, maturity, understanding of long-term effects, etc.
For both options, medical personnel have ethical standards to uphold, and need to be convinced that the child has shown a lasting pattern of gender nonconformity (the “persistent, insistent, consistent” guideline from yesterday’s post), they need to address any psychological, medical, or social problems that could interfere with the treatment, and they must be assured that the child is able to understand the treatment and agree to have it (even though the treatment requires parent/guardian consent). These treatments are not given lightly or glibly.
It’s also incredibly important to emphasize the fact that these are medical decisions made by the parents/guardians, the child, and the medical doctor. Both of these medical interventions are only administered and monitored by medical doctors and require regular check-ups, bloodwork, and careful monitoring.
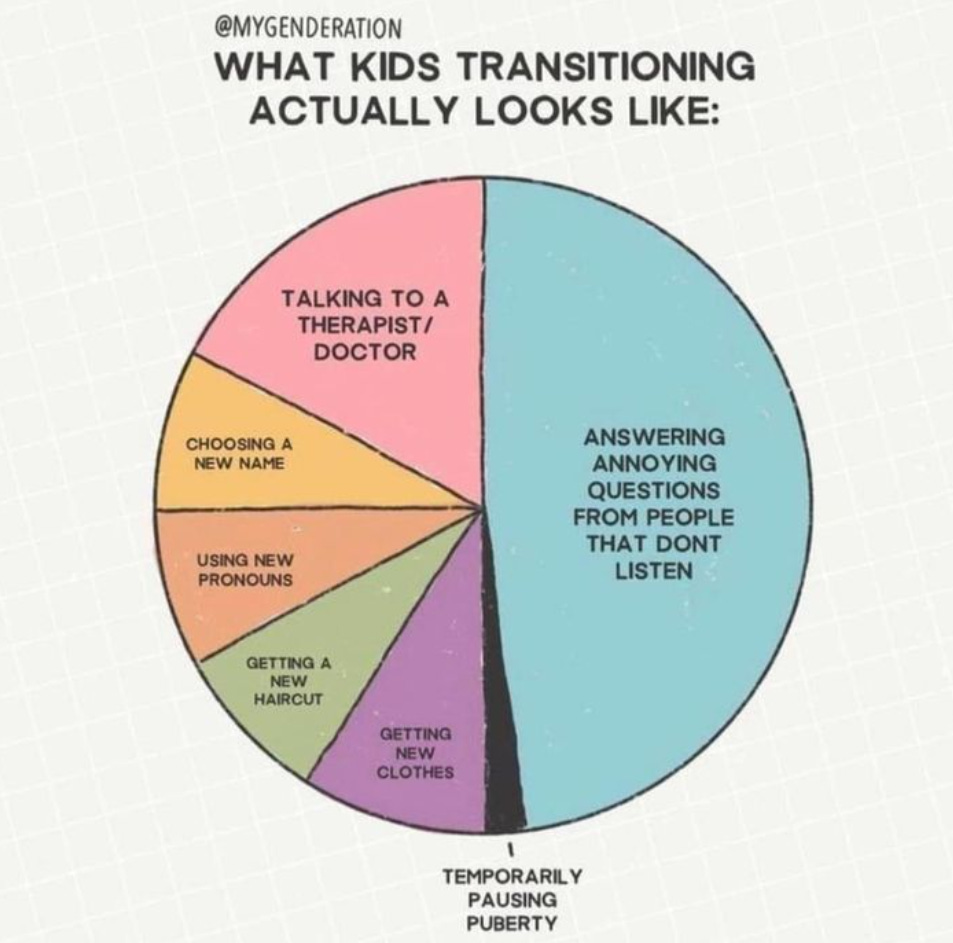
I mention this because it was apparent that some of the concerns raised at the parents' rights rallies indicated a belief that medical treatments and surgery happen at school, or that children are just able to get hormone therapy on a whim, and that is absolutely untrue.
It’s important to note that surgery is not an option for pre-adolescents and is very rarely (almost never) an option for adolescents ages 15 -17. There have been infrequent cases where the parents/guardians, the doctor, the psychologist, and the trans teen have agreed that it’s in the best interest for the teenager to have “top” surgery if the teen’s gender dysphoria is becoming life-threatening. Generally speaking, however, medical practitioners take the approach of supporting their patient’s education and encouraging them to reflect on if (or how) surgical interventions might fit into their future lives. (Please note that “bottom” or “lower” surgery is restricted to individuals aged 18 and up with no exceptions).
(Note: A GP who is well-versed in transitioning would be able to help a family and their child through this process, but the GDAAY clinic that I mentioned previously has a team of clinical experts to support transgender youth, including child and adolescent psychiatry, clinical psychology, adolescent medicine, and pediatric endocrinology. This team sees children ages 7 – 16 for new consults and follows them until they’re 17. GDAAY works with another Manitoba program – Klinic’s Trans Health program – to transition kids into adult health care at 17.)
Transitioning at ages 16 Yrs and up:
OK, so far I’ve been describing an ideal situation, where a trans child lives in a province / state where gender affirming medical care has not been politicized and is solely left in the hands of trained medical personnel, is raised in a home that offers unconditional support and acceptance of their child, and where the parents/guardians have made intentional and careful decisions along the way to ensure that their child has been given both the freedom and support to live out their inner knowing of who they are, with room to explore, adjust, change, and backtrack if necessary.
If this is the case, then nothing much really changes when a child turns 16. If they are not part of the GDAAY program and are on GAHT prescribed by their GP, they would simply continue under the guidance of their GP.
I’ll just add that this “ideal situation” of the transitioning process that I originally outlined (the version with full parental support) has been confirmed by research to be a scenario where trans children and youth thrive.
In the next post we’ll look at what transitioning looks like for trans kids who don’t have parental support.
~ K.